Understanding the risks: a practical health briefing for e-füst users
This comprehensive, user-focused report is crafted to help current and prospective e-füst users better understand the respiratory consequences highlighted by research on the effects of e cigarettes on lungs. The aim is not to repeat a title verbatim, but to translate evidence into clear, actionable information. The landscape of research has evolved rapidly, and readers deserve a concise synthesis that emphasizes what matters most for lung health, risk perception, and informed decision-making.
Why lung health is central to choosing vapor products
Breathing is fundamental. Changes to respiratory function can be subtle at first yet have meaningful long-term consequences. For anyone using e-füst devices, attention to the effects of e cigarettes on lungs is essential because inhalation delivers aerosols directly to the airway lining, where chemical and physical interactions take place immediately. Short-term irritation can progress to chronic changes if exposures persist.
Core mechanisms that link aerosol exposure to lung effects
- Inflammation: Aerosol particles and dissolved chemicals can activate immune cells in the airway, leading to inflammation that compromises gas exchange and repair processes.
- Oxidative stress:
 Certain constituents generate reactive oxygen species, damaging cells and extracellular matrix components crucial for healthy lung architecture.
Certain constituents generate reactive oxygen species, damaging cells and extracellular matrix components crucial for healthy lung architecture. - Altered immune defenses: Disruption of normal mucociliary clearance and immune signaling can increase susceptibility to infections and delay recovery after injury.
- Structural changes: Persistent injury and ineffective repair may lead to airway remodeling and reduced lung elasticity over time.
What aerosols commonly contain and why composition matters
The inhaled aerosol from devices like e-füst generally includes a vehicle (propylene glycol, vegetable glycerin), nicotine (absent in some formulations), flavoring chemicals, and thermal degradation products. Particle size distribution determines where particles deposit in the respiratory tract: ultrafine particles reach deep alveoli, while larger droplets land in conducting airways. Both deposition patterns have implications for the effects of e cigarettes on lungs because the site of deposition influences the type of injury and the cellular populations affected.
generally includes a vehicle (propylene glycol, vegetable glycerin), nicotine (absent in some formulations), flavoring chemicals, and thermal degradation products. Particle size distribution determines where particles deposit in the respiratory tract: ultrafine particles reach deep alveoli, while larger droplets land in conducting airways. Both deposition patterns have implications for the effects of e cigarettes on lungs because the site of deposition influences the type of injury and the cellular populations affected.
- Vehicles (PG/VG): hygroscopic behavior can alter airway surface liquid and mucociliary function.
- Nicotine: vasoactive and pro-inflammatory effects that may modify immune responses.
- Flavorants: some commonly used compounds are linked to airway toxicity in lab models.
- Thermal breakdown products: aldehydes and volatile organic compounds have known respiratory toxicity.
Short-term responses observed in users and volunteers
Controlled human exposure studies and observational reports typically describe immediate effects such as throat irritation, coughing, wheeze, and transient changes in airway resistance or exhaled nitric oxide—an inflammation marker. While many of these effects resolve after cessation of use, repeated exposures can maintain a pro-inflammatory state. Several studies using biomarkers (e.g., inflammatory cytokines in sputum, exhaled breath condensate) show that even short-term use alters measurable indices of airway inflammation, supporting concerns observed in symptomatic users.
Evidence from clinical, epidemiological, and experimental studies
The evidence base for the effects of e cigarettes on lungs combines diverse methodologies: population-level surveys, clinical cohorts, randomized trials (often focused on smoking cessation), and mechanistic laboratory studies using cells and animal models. Each approach contributes unique insights but also has limitations. For example, long-term randomized trials with lung outcomes are rare for ethical and logistical reasons, while observational studies must adjust for prior cigarette smoking, environmental exposures, and product variability.
Key takeaway: No single study can capture all risks. Converging lines of evidence from human, animal, and cellular research suggest that inhaling heated aerosol is not inert and can produce measurable adverse respiratory effects.
Human observational findings
- Cross-sectional analyses link e-cigarette use to higher odds of chronic bronchitic symptoms and wheeze, especially in young people.
- Dual users (those who smoke cigarettes and use e-cigarettes) often show worse respiratory symptom burden than exclusive users of either product, complicating attributions.
- Some longitudinal studies indicate an association between e-cigarette use and subsequent respiratory symptom development, though confounding remains a challenge.
Clinical and experimental signals
- Bronchoscopy and sputum studies reveal inflammatory cell recruitment after exposure and alterations in gene expression associated with stress-response pathways.
- Animal models demonstrate airway inflammation, mucus hypersecretion, and impaired host defense following repeated aerosol exposure.
- In vitro studies show cytotoxicity and impaired ciliary function with many flavoring agents and thermal degradation products, strengthening biological plausibility for observed human effects.
Vulnerable groups who should be particularly cautious
Not all users face the same level of risk. Groups requiring extra caution include adolescents (whose lungs are still developing), pregnant people (fetal lung development may be affected), those with pre-existing respiratory disease (asthma, COPD), and immunocompromised individuals. For these populations, the potential effects of e cigarettes on lungs may compound existing vulnerabilities and accelerate symptom progression.
Clinical signs that warrant medical attention
 e-füst health report – why e-füst users should care about effects of e cigarettes on lungs and what studies show” />
e-füst health report – why e-füst users should care about effects of e cigarettes on lungs and what studies show” />
Users of e-füst should seek medical evaluation if they experience persistent cough, new or worsening shortness of breath, chest tightness, recurring pneumonia, or unexplained declines in exercise tolerance. Clinicians may evaluate symptoms with spirometry, imaging, and biomarkers of inflammation according to clinical judgment.
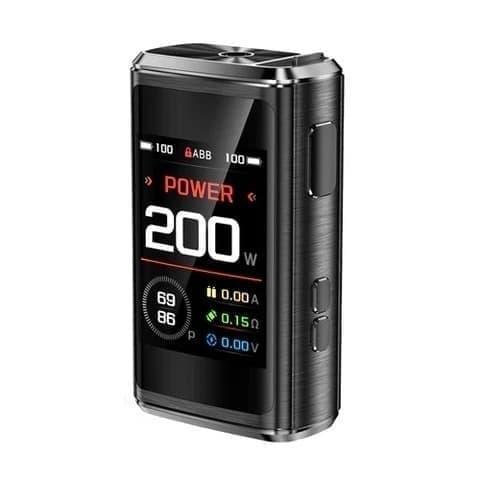
Harm reduction: how product choice and behavior influence risk
For smokers switching to e-füst devices as a risk reduction strategy, evidence suggests reduced exposure to certain combustion-related toxins. However, harm reduction does not equal risk elimination. Choices that can reduce exposure include avoiding high-temperature settings that increase thermal breakdown, choosing nicotine strengths that minimize compensatory puffing, and selecting products with fewer unnecessary flavor additives. Complete cessation of all inhaled tobacco or nicotine products remains the most protective option for lung health.
Common misconceptions and balanced clarifications
- Myth: “Vaping is harmless water vapor.” Clarification: The aerosol is a complex mixture; it is not merely water and can contain bioactive chemicals that affect airway cells.
- Myth: “Only smokers are at risk.” Clarification: Non-smokers, especially youth, who begin using e-cigarettes may develop respiratory symptoms and altered immune responses.
- Myth: “If there’s no nicotine, it’s safe.” Clarification: Many health effects stem from vehicles and flavorants independent of nicotine.
Practical guidance for users and clinicians
- Assess baseline lung health: consider spirometry for users with symptoms or prior lung disease.
- Monitor symptoms: track cough, breathlessness, sputum production, and changes in exercise capacity.
- Reduce exposure where possible: avoid unnecessary flavorants, lower device temperatures, and follow manufacturer safety recommendations.
- Consider cessation support: for those who want to stop, evidence-based behavioral and pharmacologic interventions improve success rates.
Regulatory and public health considerations
Public health authorities must balance potential benefits of less harmful alternatives for adults who smoke with the need to prevent youth uptake. Product standards that limit harmful constituents, restrict appealing flavors to youth, and enforce quality control can modify population-level harms associated with e-füst and similar products. Surveillance systems tracking respiratory outcomes among users are essential to identify emerging patterns early.
Research gaps and priorities
While substantial progress has been made, several research needs remain: long-term prospective cohort studies with detailed exposure assessment, standardized clinical outcome measures, comparative studies of different device types and formulations, and translational work linking biomarkers to clinical endpoints. Filling these gaps will refine understanding of the true magnitude and mechanisms of the effects of e cigarettes on lungs .
.
How to interpret study findings responsibly
Not all studies are equivalent. High-quality evidence typically comes from well-designed longitudinal cohorts and mechanistic studies that control for confounding factors like prior smoking. Readers should interpret single studies cautiously, particularly those with small samples, short follow-up, or limited exposure characterization. Meta-analyses that synthesize consistent findings across multiple high-quality studies provide stronger guidance on the likely long-term impact.
Summary and takeaways
For anyone using or considering e-füst: attention to respiratory health is warranted. Current research indicates that inhaled aerosols from electronic nicotine-delivery systems have biologically plausible and measurable effects on the airways and lung function. While these products may reduce exposure to some tobacco combustion byproducts for adult smokers who switch completely, they also pose their own set of risks, especially for young people and vulnerable groups. Monitoring symptoms, minimizing avoidable exposures, and seeking clinical evaluation when changes occur are practical steps users can take now.
- Regularly assess for chronic cough or breathlessness.
- Avoid high-temperature device settings and unknown refill liquids.
- Keep product use age-appropriate policies in mind and prevent youth access.
- Discuss cessation or harm reduction strategies with a healthcare provider if concerned.
Evidence-informed resources
Reputable sources for ongoing information include peer-reviewed journals focused on respiratory medicine, public health agency reports, and clinical guidelines produced by professional respiratory societies. These sources synthesize evolving data on the effects of e cigarettes on lungs and translate them into practice recommendations.
Final remarks for readers
Knowledge empowers safer choices. Whether you are a long-term user, a recent switcher from combustible cigarettes, a clinician, or a concerned family member, understanding how inhaled aerosols interact with lung biology helps frame decisions about product use and health monitoring. The balance of evidence underscores caution: inhaling aerosolized chemicals is not risk-free, and vigilance around respiratory symptoms is prudent for all e-füst users.
Frequently Asked Questions (FAQ)
- Q: Can vaping cause permanent lung damage?
- A: Studies indicate that repeated airway injury and inflammation can lead to structural changes over time, but the magnitude of permanent damage depends on exposure duration, product composition, individual susceptibility, and smoking history. More long-term data are needed to quantify risks precisely.
- Q: Is switching to e-füst safer than continuing to smoke cigarettes?
- A: For adult smokers who switch completely, many harmful combustion-related exposures decline. However, complete elimination of risk is not guaranteed, and the best way to protect lung health remains complete cessation of all inhaled nicotine and tobacco products.
- Q: Are flavored products more harmful to the lungs?
- A: Some flavoring chemicals have shown airway toxicity in laboratory studies. While not all flavors pose the same risk, flavorants add chemical complexity and have been implicated in adverse effects in preclinical models.
Note: This article synthesizes current scientific understanding without providing individualized medical advice. If you experience new or worsening respiratory symptoms, consult a healthcare professional for personalized assessment and care.